Ethnomedicinal survey and in-vitro antibacterial screening of medicinal plants used in treatment of wounds in Ijesha land, South-Western Nigeria
*Article not assigned to an issue yet
Ogundele Seun B., Olorunmola Felix O., Agbedahunsi Joseph M.
Research Articles | Published: 09 May, 2025
First Page: 0
Last Page: 0
Views: 741
Keywords: Antibacterial activities, Bacterial infections in wounds, Ethnomedicinal survey, Ijesha land, Medicinal plants
Abstract
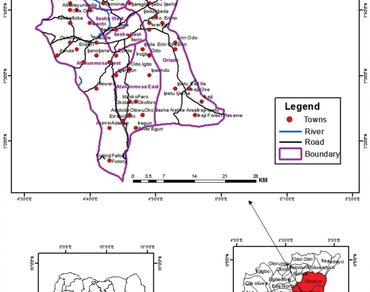
This paper documented medicinal plants used by Traditional Medical Practitioners in Ijesha land for the treatment of wounds and evaluated their antibacterial activities. Semi-structured questionnaire was used to gather information about medicinal plants used in the treatment of wound infections by Traditional Medical Practitioners among the Ijesha ethnic group of the Yoruba tribe. The medicinal plants encountered were analysed using ethnomedicinal indices. Hydroethanolic extract of 22 selected plants was prepared by maceration at room temperature with 80% EtOH: H2O for 48 h, evaporated under reduced pressure and lyophilized. The antibacterial activities of the plant extracts against standard microorganisms were carried out using agar well diffusion and dilution methods. Eighty-four medicinal plants were identified. The extracts exhibited good antibacterial activity against one or more of the tested organisms. S. aureus was susceptible to 18 plant extracts, The MIC values ranged from 0.47 to 3.75 mg/mL, while leaf extracts of Bidens pilosa, Phragmanthera capitata, and Dalbergiella welwitschii were not active against S. aureus. Artocarpus altilis stem bark extract showed good antibacterial activity against gram-negative organisms with a mean zone of inhibition of 19.7 ± 0.37, 14.0 ± 1.52, 15.7 ± 0.85, 13.3 ± 1.20, 12.7 ± 0.35 mm against K. pneumoniae, E. coli, P. vulgaris, S. marcenscens and P. aeruginosa .respectively. Proteus vulgaris was resistant to 11 of the plant extracts tested, followed by P. aeruginosa (10) as against E. coli (4). Leaf extracts of Croton zambesicus, Dalbergiella welwitschii, S. alata, and A. altilis stem bark showed pronounced activity against M. luteus with a mean zone of inhibition of 14.7 ± 4.63, 17.7 ± 0.69, 16.0 ± 0.00, 15.0 ± 0.00 mm and MIC values of 1.88, 0.47, 0.47, 0.47 mg/mL respectively. These findings justify the use of medicinal plants in ethnomedicine for the treatment of wounds infections among the Ijesha people of Southwestern Nigeria.
References
Abrahamian FM, Goldstein EJ (2011) Microbiology of animal bite wound infections. Clin Microbiol Rev 24(2):231–246. https://doi.org/10.1128/CMR.00041-10PMID: 21482724, PMCID: PMC3122494
Aggarwal R, Mahajan P, Pandiya S, Bajaj A, Verma SK, Yadav P, Kharat AS, Khan AU, Dua M, Johri AK (2024) Antibiotic resistance: a global crisis, problems and solutions. Crit Rev Microbiol 50(5):896–921 Epub 2024 Feb 21. PMID: 38381581
Al-mariri A, Safi M (2014) In vitro antibacterial activity of several plant extracts and oils against some Gram-negative Bacteria. Iran J Med Sci 39(1):36–43 PMID: 24453392; PMCID: PMC3895893
Aswathanarayan JB, Rao P, Hm S, Gs S, Rai RV (2023) Biofilm-Associated infections in chronic wounds and their management. Adv Exp Med Biol 1370:55–75. https://doi.org/10.1007/5584_2022_738. PMID: 36251248
Awoyemi OK, Abdulkarim IA, Ewa EE, Adeloju RA (2012) Ethnobotanical assessment of herbal plants in South-western Nigeria. Acad Res Int 2(3):50–57
Ayeni EA, Aliyu N (2018) Ethnomedicinal survey and Documentation of healing river sources among the Yoruba people (Ijesha land) Nigeria. J Complement Med Res 8(2):59–70
Bamisaye FA, Ajani EO, Minari JB (2013) Medicinal plants studies prospects of ethnobotanical uses of pawpaw (Carica papaya). J Med Plants Stud 1(4):171–177
Barbalho SM, Araújo AC, Penteado Detregiachi CR, Buchaim DV, Guiguer ÉL (2019) The potential role of medicinal plants in bone regeneration. Altern Ther Health Med Jul 25(4):32–39 PMID: 31202209
Brinkac L, Voorhies A, Gomez A, Nelson KE (2017) The threat of antimicrobial resistance on the human Microbiome. Microb Ecol Nov 74(4):1001–1008. https://doi.org/10.1007/s00248-017-0985-zEpub 2017 May 11. PMID: 28492988; PMCID: PMC5654679
Burillo A, Pulido-Pérez A, Bouza E (2024) Current challenges in acute bacterial skin infection management. Curr Opin Infect Dis. 37(2):71–79. https://doi.org/10.1097/QCO.0000000000000989. Epub 2024 Jan 3. PMID: 38179868
Burnashov SI, Shipitsyna IV, Osipova EV (2019) Microflora of surgical wounds and fistulas in patients with chronic osteomyelitis of the tibia before reconstructive treatment, in case of recurrence of infection. Klin Lab Diagn 64(10):627–631. https://doi.org/10.18821/0869-2084-2019-64-10-627-631. Russian
Cavallo I, Sivori F, Mastrofrancesco A, Abril E, Pontone M, Di Domenico EG, Pimpinelli F (2024) Bacterial biofilm in chronic wounds and possible therapeutic approaches. Biology (Basel) 13(2):109. https://doi.org/10.3390/biology13020109PMID: 38392327; PMCID: PMC10886835
Cepas V, Soto SM (2020) Relationship between virulence and resistance among gram-negative bacteria. Antibiot (Basel) 9(10):719. https://doi.org/10.3390/antibiotics9100719PMID: 33092201; PMCID: PMC7589547
Coker ME, Oaikhena AO (2020) Antimicrobial activity of the crude extracts and fractions of Ficus thonningii (Blume) on isolates from urinary tract infections. J Medicinally Act Plants 9(4):310–332
Derakhshanfar A, Moayedi J, Derakhshanfar G, Poostforoosh Fard A (2019) The role of Iranian medicinal plants in experimental surgical skin wound healing: an integrative review. Iran J Basic Med Sci Jun 22(6):590–600. https://doi.org/10.22038/ijbms.2019.32963.7873PMID: 31231485; PMCID: PMC6570749
Dike IP, Obembe OO, Adebiyi EF (2012) Ethnobotanical survey for potential Anti-Malarial plants in South-western Nigeria. J Ethnopharmacol 144(3):618–626
El-Ashram S, El-Samad LM, Basha AA, El Wakil A (2021) Naturally-derived targeted therapy for wound healing: beyond classical strategies. Pharmacol Res Aug 170:105749. https://doi.org/10.1016/j.phrs.2021.105749Epub 2021 Jun 30. PMID: 34214630
Ferri M, Ranucci E, Romagnoli P, Giaccone V (2017) Antimicrobial resistance: A global emerging threat to public health systems. Crit Rev Food Sci Nutr. Sep 2;57(13):2857–2876. https://doi.org/10.1080/10408398.2015.1077192. PMID: 26464037
Gerada A, Harper N, Howard A, Reza N, Hope W (2024) Determination of minimum inhibitory concentrations using machine-learning-assisted agar dilution. Microbiol Spectr. 12(5):e0420923. https://doi.org/10.1128/spectrum.04209-23. Epub 2024 Mar 22. PMID: 38517194; PMCID: PMC11064640
Glik J, Kawecki M, Gazdzik T, Nowak M (2012) The impact of the types of microorganisms isolated from blood and wounds on the results of treatment in burn patients with sepsis. Pol Przegl Chir 84(1):6–16. https://doi.org/10.2478/v10035-012-0002-7PMID:22472489
Grierson DS, Afolayan AJ (1999) An ethnobotanical study of plants used for the treatment of wounds in the Eastern cape, South Africa. J Ethnopharmacol 67:327–332
He H, Li A, Li S, Tang J, Li L, Xiong L (2021) Natural components in sunscreens: topical formulations with sun protection factor (SPF). Biomed Pharmacother 134:111161. https://doi.org/10.1016/j.biopha.2020.111161Epub 2020 Dec 24. PMID: 33360043
Jiang B, Lai Y, Xiao W, Zhong T, Liu F, Gong J, Huang J (2024) Microbial extracellular vesicles contribute to antimicrobial resistance. PLoS Pathog 20(5):e1012143. https://doi.org/10.1371/journal.ppat.1012143PMID: 38696356; PMCID: PMC11065233
Karabay O, Teker B (2010) Burn wounds and microorganisms. Burns 36(1):141–142. https://doi.org/10.1016/j.burns.2009.02.026, PMID: 19857926
Karinja SJ, Spector JA (2018) Treatment of Infected Wounds in the Age of Antimicrobial Resistance: Contemporary Alternative Therapeutic Options. Plast Reconstr Surg. Oct;142(4):1082–1092. https://doi.org/10.1097/PRS.0000000000004799. PMID: 30252823
Khan I, AbdElsalam MN, Fouad H, Tariq A, Ullah R, Adnan M (2014) Application of ethnobotanical indices on the use of traditional medicines against common diseases. Evidence-Based Complement Altern Med 635371:1–21
Liu Y, Long S, Wang H, Wang Y (2024) Biofilm therapy for chronic wounds. Int Wound J 21(2):e14667. https://doi.org/10.1111/iwj.14667PMID: 38339793; PMCID: PMC10858329
Mayer DO, Tettelbach WH, Ciprandi G, Downie F, Hampton J, Hodgson H, Lazaro-Martinez JL, Probst A, Schultz G, Stürmer EK, Parnham A, Frescos N, Stang D, Holloway S, Percival SL (2024) Best practice for wound debridement. J Wound Care. 33(Sup6b):S1-S32. https://doi.org/10.12968/jowc.2024.33.Sup6b.S1. PMID: 38829182
McEwen SA, Collignon PJ (2018) Antimicrobial Resistance: a One Health Perspective. Microbiol Spectr. Mar;6(2). https://doi.org/10.1128/microbiolspec.ARBA-0009-2017. PMID: 29600770
Meenu MT, Kaul G, Akhir A, Shukla M, Radhakrishnan KV, Chopra S (2022) Developing the natural Prenylflavone Artocarpin from Artocarpus hirsutus as a potential lead targeting pathogenic, Multidrug-Resistant Staphylococcus aureus, persisters and biofilms with no detectable resistance. J Nat Prod 85(10):2413–2423. https://doi.org/10.1021/acs.jnatprod.2c00621Epub 2022 Oct 12. PMID: 36222797
Meenu MT, Kaul G, Shukla M, Radhakrishnan KV, Chopra S (2021) Cudraflavone C from Artocarpus hirsutus as a promising inhibitor of pathogenic, Multidrug-Resistant S. aureus, persisters, and biofilms: A new insight into a rational explanation of traditional wisdom. J Nat Prod 84(10):2700–2708. https://doi.org/10.1021/acs.jnatprod.1c00578Epub 2021 Sep 21. PMID: 34546736
Morrison L, Zembower TR (2020) Antimicrobial resistance. Gastrointest endosc clin N am. 30(4):619–635. https://doi.org/10.1016/j.giec.2020.06.004. Epub 2020 Aug 1. PMID: 32891221
Nierenberg NE, Levine JM (2024) Infectious Aspects of Chronic Wounds. Clin Geriatr Med. 40(3):471–480. https://doi.org/10.1016/j.cger.2024.03.001. Epub 2024 Apr 12. PMID: 38960538
Nigussie D, Makonnen E, Tufa TB, Brewster M, Legesse BA, Fekadu A, Davey G (2021) Systematic review of Ethiopian medicinal plants used for their anti-inflammatory and wound healing activities. J Ethnopharmacol. Aug 10;276:114179. https://doi.org/10.1016/j.jep.2021.114179. Epub 2021 May 11. PMID: 33989738
Ogundele SB, Oriola AO, Oyedeji AO et al (2022) Flavonoids from stem bark of Artocarpus altilis (Parkinson ex F.A.Zorn) Fosberg. Chem Afr 5:1921–1935. https://doi.org/10.1007/s42250-022-00489-z
Okeke IN, de Kraker MEA, Van Boeckel TP, Kumar CK, Schmitt H, Gales AC, Bertagnolio S, Sharland M, Laxminarayan R (2024) The scope of the antimicrobial resistance challenge. Lancet. 403(10442):2426–2438. https://doi.org/10.1016/S0140-6736(24)00876-6. Epub 2024 May 23. Erratum in: Lancet. 2024;404(10457):1018. https://doi.org/10.1016/S0140-6736(24)01879-8. PMID: 38797176
Olaru ID, Schoeler S, Schaumburg F (2024) The impact of agar depth on antimicrobial susceptibility testing by disc diffusion. J Med Microbiol 73(9):001890. https://doi.org/10.1099/jmm.0.001890PMID: 39292220; PMCID: PMC11410041
Olasunkanmi OO, Akinpelu DA, Adeniyi PO, Ajayi OF, Joseph Omololu-Aso, Olorunmola FO (2017) Investigations into antimicrobial, phytochemnical and antioxidant properties of Vitellaria paradoxa (Gaertn.) stem bark extracts. J Pharm Res Int 20(5):1–17. https://doi.org/10.9734/JPRI/2017/38749
Olorunisola OS, Adetutu A, Balogun EA, Afolayan AJ (2013) Ethnobotanical survey of medicinal plants used in the treatment of malarial in Ogbomoso, Southwest Nigeria. J Ethnopharmacol 150:71–78
Olorunnisola SO, Adetutu A, Afolayan AJ (2015) An inventory of plants used in the treatment of some disease conditions in Ogbomoso, Southwest, Nigeria. J Ethnopharmacol 161:60–68
Polerà N, Badolato M, Perri F, Carullo G, Aiello F (2019) Quercetin and its Natural Sources in Wound Healing Management. Curr Med Chem.;26(31):5825–5848. https://doi.org/10.2174/0929867325666180713150626. PMID: 30009700
Pranantyo D, Yeo CK, Wu Y, Fan C, Xu X, Yip YS, Vos MIG, Mahadevegowda SH, Lim PLK, Yang L, Hammond PT, Leavesley DI, Tan NS, Chan-Park MB (2024) Hydrogel dressings with intrinsic antibiofilm and antioxidative dual functionalities accelerate infected diabetic wound healing. Nat Commun 15(1):954. https://doi.org/10.1038/s41467-024-44968-yPMID: 38296937; PMCID: PMC10830466
Proft T, Baker EN (2009) Pili in gram-negative and gram-positive bacteria-structure, assembly and their role in disease. Cell Mol Life Sci 66(4):613–635. https://doi.org/10.1007/s00018-008-8477-4, PMID: 18953686
Punjataewakupt A, Napavichayanun S, Aramwit P (2019) The downside of antimicrobial agents for wound healing. Eur J Clin Microbiol Infect Dis. Jan;38(1):39–54. https://doi.org/10.1007/s10096-018-3393-5. Epub 2018 Oct 5. PMID: 30291466
Rahim K, Saleha S, Zhu X, Huo L, Basit A, Franco OL (2017) Bacterial Contribution in Chronicity of Wounds. Microb Ecol. 2017;73(3):710–721. https://doi.org/10.1007/s00248-016-0867-9. Epub Oct 14. PMID: 27742997
Rajoo A, Ramanathan S, Mansor SM, Sasidharan S (2021) Formulation and evaluation of wound healing activity of Elaeis guineensis Jacq leaves in a Staphylococcus aureus infected Sprague Dawley rat model. J Ethnopharmacol. 2021;266:113414. https://doi.org/10.1016/j.jep.2020.113414. Epub 2020 Sep 24. PMID: 32980488
Ruhal R, Sahu A, Koujalagi T, Das A, Prasanth H, Kataria R (2024) Biofilm-specific determinants of enterococci pathogen. Arch Microbiol. 206(10):397. https://doi.org/10.1007/s00203-024-04119-9. PMID: 39249569
Rupp M, Walter N, Bärtl S, Heyd R, Hitzenbichler F, Alt V (2024) Fracture-Related Infection-Epidemiology, etiology, diagnosis, prevention, and treatment. Dtsch Arztebl Int 121(1):17–24. https://doi.org/10.3238/arztebl.m2023.0233PMID: 37970721; PMCID: PMC10916768
Septimus EJ (2018) Antimicrobial resistance: an antimicrobial/Diagnostic stewardship and infection prevention approach. Med Clin North Am 102(5):819–829. https://doi.org/10.1016/j.mcna.2018.04.005Epub 2018 Jun 27. PMID: 30126573
Sharifi-Rad J, Butnariu M, Ezzat SM, Adetunji CO, Imran M, Sobhani SR, Tufail T, Hosseinabadi T, Ramírez-Alarcón K, Martorell M, Maroyi A, Martins N (2020) Mushrooms-Rich preparations on wound healing: from nutritional to medicinal attributes. Front Pharmacol Sep 16:11:567518. https://doi.org/10.3389/fphar.2020.567518PMID: 33041809; PMCID: PMC7525158
Shedoeva A, Leavesley D, Upton Z, Fan C (2019) Wound Healing and the Use of Medicinal Plants. Evid Based Complement Alternat Med. Sep 22;2019:2684108. https://doi.org/10.1155/2019/2684108. PMID: 31662773; PMCID: PMC6778887
Shettigar K, Murali TS (2020) Virulen factors and Clonal diversity of Staphylococcus aureus in colonisation and wound infection with emphasis on diabetic foot infection. Eur J Clin Microbiol Infect Dis. 2020;39(12):2235–2246. https://doi.org/10.1007/s10096-020-03984-8. Epub 2020 Jul 18. PMID: 32683595; PMCID: PMC7669779
Tangcharoensathien V, Cars O, Lekagul A (2024) The 2024 political declaration on antimicrobial resistance needs bold targets. BMJ. 386:q2084. https://doi.org/10.1136/bmj.q2084. PMID: 39322251
Tyavambiza C, Dube P, Goboza M, Meyer S, Madiehe AM, Meyer M (2021) Wound Healing Activities and Potential of Selected African Medicinal Plants and Their Synthesized Biogenic Nanoparticles. Plants (Basel). Nov 30;10(12):2635. https://doi.org/10.3390/plants10122635. PMID: 34961106; PMCID: PMC8706794
Uberoi A, McCready-Vangi A, Grice EA (2024) The wound microbiota: microbial mechanisms of impaired wound healing and infection. Nat Rev Microbiol. 22(8):507–521. https://doi.org/10.1038/s41579-024-01035-z. Epub 2024 Apr 4. PMID: 38575708
Usman IA, Olawore NO, Oladosu I, Hamid AA, Elaigwu SE (2009) Constituents of leaf oil of Croton zambesicus muell.arg growing in North central Nigeria. Middle-East J Sci Rep 4(4):242–244
Uwamino Y, Aoki W, Inose R, Kamoshita Y, Mikita K, Namkoong H, Nishimura T, Matsushita H, Hasegawa N (2024) Minimum inhibitory concentrations of Azithromycin in clinical isolates of Mycobacterium avium complex in Japan. Microbiol Spectr 12(6):e0021824. https://doi.org/10.1128/spectrum.00218-24Epub 2024 Apr 30. PMID: 38687080; PMCID: PMC11237530
Villa F, Marchandin H, Lavigne J-P, Schuldiner S, Cellier N, Sotto A, Loubet P (2024) Anaerobes in diabetic foot infections: pathophysiology, epidemiology, virulence, and management. Clin Microbiol Rev 37(3):e0014323. https://doi.org/10.1128/cmr.00143-23Epub 2024 May 31. PMID: 38819166; PMCID: PMC11391693
Wilcox M, Benoit-Vical F, Fowler D, Bourdy G, Burford G, Giani S, Graziose R, Houghton P, Randrianarivelojosia M, Rasoanaivo P (2011) Do ethnobotanical and laboratory data predict clinical safety and efficacy of Anti-Malarial plants?? Malarial J 10(1):S1–S7
Yazarlu O, Iranshahi M, Kashani HRK, Reshadat S, Habtemariam S, Iranshahy M, Hasanpour M (2021) Perspective on the application of medicinal plants and natural products in wound healing: A mechanistic review. Pharmacol Res Dec 174:105841. https://doi.org/10.1016/j.phrs.2021.105841Epub 2021 Aug 20. PMID: 34419563
Author Information
Department of Pharmacognosy and Natural Products, College of Pharmacy, Afe Babalola University, Ado-Ekiti, Nigeria